Do You Want To Beat Endo & Get Your Life Back?
World Class Robotic Surgery And Integrative Healing
Endometriosis Treatment
Dr Steven Vasilev
MD, FACOG, FACS, FACN, ABOIM

About Endometriosis
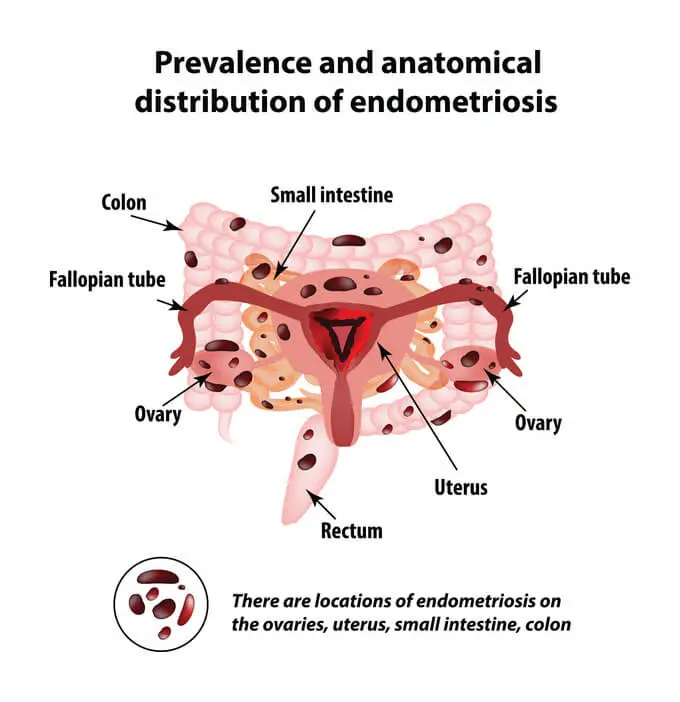
Endometriosis is extremely common, affecting as many as 1 in 10 women. Yet it is extremely underdiagnosed, leading to unnecessary pain and suffering for years. Endo occurs when the tissue that normally lines the inside of the uterus (endometrium) grows outside of it inside your pelvis and abdomen. Endometriosis implant cells and endometrial cells that are normally inside the uterus are NOT the same from a molecular biology point of view. These significant differences provide an opportunity for targeted therapy development. Research is in progress, but the answer has been elusive.
Endometriosis is extremely common, affecting as many as 1 in 10 women. Yet it is extremely underdiagnosed, leading to unnecessary pain and suffering for years. Endo occurs when the tissue that normally lines the inside of the uterus (endometrium) grows outside of it inside your pelvis and abdomen. Endometriosis implant cells and endometrial cells that are normally inside the uterus are NOT the same from a molecular biology point of view. These significant differences provide an opportunity for targeted therapy development. Research is in progress, but the answer has been elusive.
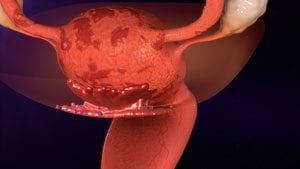
The exact cause of endometriosis remains unknown, but most theories center on how one’s cells, hormones and immune system works. It may also be due to ectopic endometrial tissue, aberrant endocrine signaling or genetic factors. It’s definitely not a simple answer. It is possible that more than one cause exists and we know that even newborns can have endometriosis. Women can develop endometriomas, or “chocolate cysts” with old blood produced by endometriosis tissue that grows on and in the ovary.
Pelvic endometriosis can be categorized as superficial peritoneal, ovarian or deeply infiltrating. These lesions contain fibrous tissue, cysts and blood in addition to endometrial glands and stoma (supporting tissue). The sizes of the lesions vary. It can cause painful periods, infertility, pain during intercourse and excessive vaginal bleeding. Less common symptoms include bowel and bladder dysfunction, low back pain or chronic fatigue. Severe pain does not always equal severe endometriosis. Some patients have minimal pain with a large amount of disease and vice versa, where small but potentially deep infiltrating areas cause debilitating life-changing pain.
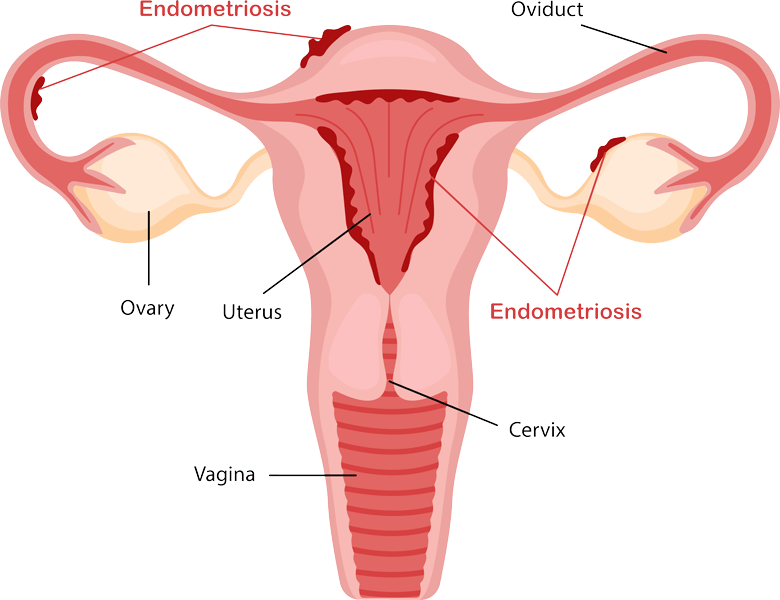
Major Subtypes
-

Superficial endometriosis (on surface)
-

Deep Infiltrating endometriosis (invading tissues)
-

Ovarian endometriosis (endometrioma)
-

Metastatic endometriosis (spread to other areas)
Endometriosis can affect not only your pelvic organs and delicate structures, which include your bladder, ureters and rectum, but also outside your pelvis higher up in the abdomen. There it can involve your intestines. Endometriosis can spread literally anywhere in your body, including, rarely, to distant organs like the lungs (metastatic).
Endometriosis Critical Tip
It’s crucially important to get the diagnosis straight and get it right early. If you have pelvic pain, at any age, do not “grin and bear it” with no answers from your doctor. Get a second opinion. If it looks like you have endo, the earlier endometriosis treatment starts, with or without minimally invasive or robotic surgery excision, the better the outcomes and the faster you can get back to a good quality of life!
Endometriosis Factoids
Very common yet under-diagnosed
10% or 1 in 10 women affected
Possibly preventable
Diet, exercise, fitness can reduce excess estrogen which may reduce growth and progression of endometriosis
Integrative holistic support
Endometriosis symptoms may be reduced by herbals and spices
Diagnosis
Biopsy is the only way to diagnose endometriosis. Imaging and biomarkers MAY help plan treatment.
Treatment
Endo is best treated with a combination of medical/hormonal and surgical approaches.
Surgical excision
Best surgery for endometriosis is excision of implants using minimally invasive surgery with laparoscopy or robotic surgery.
Best endometriosis surgeons
Type of surgeon you need depends on your situation and might include an experienced gynecologist, reproductive endocrinologist, endo-excision surgeon and a gynecologic oncologist. The more advanced the disease may be, the more a gynecologic oncologist is essential to your best endo excisional surgery outcomes. A master surgeon who has advanced robotic surgery skills and who understands the principles and practice of endometriosis excision is crucial to your success and healing.
Endometriosis Prevention and Detection
While the near future may bring molecular genetic insights into targeted prevention, today there is no reliable way to prevent endometriosis. In fact, there is a genetic predisposition which is not well understood. If you have a relative with endo, you have a 5-7x risk of being affected. What those genetic switches are will be uncovered soon and prevention and treatment will be enhanced. Meanwhile, you can do a lot towards reducing the chances it will affect you and maybe decrease endometriosis progression. The following are integrative insights into endometriosis reducing lifestyle modifications and is as natural a strategy for endometriosis treatment as possible.
Regular Exercise
Through regular intensive workouts, you’ll be able to “whip yourself into shape” and most importantly, get to a low percentage of body fat (low BMI or body mass index). By reducing the amount of body fat less estrogen is made in those fat cells and you reduce the total amount of estrogen circulating in your body. Since estrogen feeds endometriosis, the less estrogen circulating in your body, within physiologic normal limits, the better. To emphasize, the best exercise for this is high-intensity interval training (HIIT) or “burst training”. Ideally, you should work with a personal trainer or someone in the gym for safety, but you basically want to go all out for 30 seconds and then rest for 90 seconds and then repeat over and over. This type of exercise builds muscle, which burns more calories from your diet and increases human growth hormone (HGH).
Whole food plant based diet
By eating lots of vegetables as the “base” of your diet, rather than sugar and relative junk, you will lose weight and reduce the estrogen in your body through less fat production as well as helping you maintain regular cycles. When your cycles are regular there is less chance that your body is in estrogen overload. The best animal protein is wild-caught fish like salmon. Maintaining healthy fiber in your diet also helps bind and flush excess estrogen.
In this video actress Tia Mowry explains endometriosis, and how dietary changes helped her. You should consider all of this in your overall treatment and prevention strategy.
Reduce Alcohol
Unfortunately, alcohol causes estrogen spikes in your body. So, limit the drinking.
This is also a good cancer prevention strategy over the long run.
Reduce Caffeine
Similar to alcohol, consuming a lot of caffeinated drinks per day (more than one) can cause estrogen levels to rise.
So, limit this or look for less caffeinated solutions like some teas.
Avoid Xenoestrogens
We are exposed to more than 30,000 toxins per year. Some of these can act as estrogens on your body and disrupt normal hormone function. Sources include commercially raised meat and dairy products (especially processed meats), products with insecticide or pesticide residue, unfiltered tap water, many food additives and personal items such as conditioners, lotions, shampoos, soaps and even toothpastes.
Avoid soy?
This is controversial and, GMO arguments aside, the plant estrogens in soy can theoretically stimulate endo growth. Generally, you would have to consume gallons of it, but at least limiting soy products may help reduce total estrogen in your body. The scientific counter-argument to this is that plant estrogens stimulate another part of the estrogen receptor on normal and abnormal cells (cancer or endometriosis) and may actually BLOCK the effect of regular estrogen. So the jury is still out on this concept and there may be a mixed effect.
Consume Seaweed
This is not proven but also has VERY little downside. Seaweeds, like bladderwrack, may have anti-cancer properties, including anti-estrogen effects. Japanese women have among the lowest rates of breast, endometrial, and ovarian cancers, as well as longer menstrual cycles and lower estrogen levels circulating in their blood. Small animal studies and case reports in women suggest that this may alleviate some endometriosis pain due to a reduction of circulating estrogen levels.
Endometriosis Diagnosis
Diagnostic Scans and Biopsies
Imaging scans (Ultrasound, CT, MRI) are normal too often unless there is a pelvic mass which can possibly be an endometrioma. This is one of the reasons that diagnosis in the United States can be delayed by many years, if not decades, after the onset of symptoms. If you have persistent pelvic pain with normal scans, it is possible that you have endometriosis. The physical examination and detailed history of pain and overall assessment is important in helping determine if surgery should be performed for a diagnosis by biopsy.
Excision (biopsy) of an implant during minimally invasive surgery is the only way to make a certain diagnosis of endometriosis.
Rarely, a needle biopsy guided by ultrasound or CT scan can make the diagnosis. The reason it is rare is that a needle is very small and even if you place the needle accurately in an abnormal area seen on imaging the amount of biopsy tissue is tiny. The pathologist may simply find inflammation and fibrosis or scarring and no active endometriosis. This does not mean it is not there and was only millimeters away from the area the needle biopsied.
Endometriosis Biomarkers
Some blood tests, like the CA-125 “ovarian cancer tumor marker”, may be elevated in endo.
This does NOT mean you have cancer because CA-125 can be elevated in any inflammatory disease.
Endometriosis is inflammatory.
With the advent of “omics”, including genomics, metabolomics, proteomics and other research areas, promising blood tests are being developed.
So far, none are accurate enough to help in the diagnosis or follow-up testing of endometriosis.
Endometriosis Treatment
Treatment of endometriosis is partly dependent on where it is located (pelvis or outside the pelvis) and what the stage is. Staging is a classification of the severity of pelvic endo.
Stages of Endometriosis:
According to ASRM (American Society of Reproductive Medicine), there are four stages of pelvic endometriosis. This does not always correlate with the symptoms. Someone can have high stage and less pain than another person with lower stage and more pain. But this staging helps determine treatment and the type of surgery that might be best for you. The following is simplified but the general groupings are as listed.

Stage I
Minimal Endometriosis
There are small patches or implants either on or around the organs in the pelvis.
Stage II
Mild Endometriosis
There are more implants than in Stage I but damage to the pelvic organs is still pretty minimal and there’s not much scarring or adhesions. Altogether, when summed up the implants are not more than 5cm (couple of inches).

Stage III
Moderate Endometriosis
Implants are more widespread and are beginning to infiltrate (grow into or invade) the organs in the pelvic region, including pelvic side walls (where the blood vessels, major nerves and ureters are located) and peritoneum. There is more scarring and adhesions and endometriomas (“chocolate cyts”) of old blood in a blister on the ovary, can be seen.
Stage IV
Severe Endometriosis
The disease is definitely infiltrating or growing into and affecting several organs in the pelvic region as well as the ovaries. This may be the bladder or the rectum. Anatomy is severely distorted with scars and adhesions and there is fibrosis (like concrete) between organs. Larger and more endometriomas can be seen.
Endometriosis Surgical Treatment
Surgery for endometriosis is used for two reasons:
Diagnosis of endometriosis and
Treatment of endometriosis
Treatment is either for pain, for a suspicious pelvic mass (possible endometrioma) that might be a tumor, or for reproductive concerns like infertility. Using minimally invasive surgery through very small incisions you can get to the bottom of your pain and to make a definitive diagnosis of endometriosis. Without biopsy proof, you may be getting treated for the wrong disease. Also, early excision of significant implants can go a long way towards years of symptom-free life. Having mentioned that, it is important for your surgeon to use surgery within a well-defined strategy and to time the surgery properly. Each time surgery is done more scars can develop and the more risky the next surgery becomes. So, while this can be a phenomenal help, surgery is not without risk and this has to be balanced against the benefits you might get from it at any given point in time..

What type of surgeon for endometriosis?

The type of surgeon you need for endometriosis treatment depends on your individual situation. Are you trying to determine if you have endometriosis? Do you know you have endometriosis from prior surgery and biopsies and it’s back, causing pain? Do you have a pelvic mass that may be an endometrioma but your doctor is unsure? Do you have fertility issues and are trying to get pregnant? These may all be related but are all different in terms of the type of surgeon you need or what team of surgeons you need.
In general, to get a correct diagnosis a general gynecologist can often do that. However, if you are being treated without biopsy proof of endo, get a second opinion with either a reproductive endocrinologist (a subspecialty of ObGyn) or a fellowship trained endometriosis surgeon. If you know you have endo and need an excisional surgery for endometriosis treatment, consider a fellowship-trained gynecologic endo surgeon and/or a gynecologic oncologist. The more the disease is advanced and the more the pelvis is likely to be very scarred and anatomy distorted, a gynecologic oncologist should be involved for the treatment of endometriosis.
Why should a “cancer surgeon”, a gynecologic oncologist, be involved in endometriosis treatment? Because gynecologic oncologists have an advanced skill set to operate not only on gynecologic organs but also on surrounding intestine, rectum, ureters and bladder; all of which can be affected with endometriosis in advanced cases. Also, endometriosis is associated with an increased risk of ovarian cancer as well as degeneration of endometriosis itself to clear cell cancer or sarcoma. These are things you do not want missed and are especially important to be evaluated for as you get older with a diagnosis of endometriosis. Your life is worth at least an opinion about all of this sooner than later from the right expert, a gynecologic oncologist.
If your main concern is about fertility issues with a diagnosis of endometriosis, a reproductive endocrinologist’s opinion would be very helpful. We can help you find the right specialist if we are not the right fit for your needs. We collaborate and work with many general gynecologic surgeons, fellowship-trained excisional surgeons, and reproductive endocrinologists to help you build your team to beat your endo. We also provide integrative holistic support and can guide you in this regard as well.
Laparoscopic Excision
Minimally invasive surgery starts with laparoscopy, or “keyhole” surgery through small incisions instead of a big vertical or horizontal “bikini cut” C-section type of incisions. A camera instrument and operating instruments are inserted through these incisions, which can number from one belly button incision to four or more, depending on how many and what type of instruments are required. The instruments are scissors and graspers that are “straight stick”, which means they can only open and close in one direction. This is reasonable for relatively easy endometriosis surgery excisions but lacks finesse for more difficult surgery with advanced endometriosis and scarring.
The laparoscopic camera usually used is pretty sophisticated and offers good visibility, but in most cases lacks 3-D (three-dimensional) view and is not generally able to be magnified. In some centers, 3-D laparoscopy with magnification is available but not very common. Why is this critically important? It is not possible to predict how bad the endometriosis will be or how much scarring there is or what organs might be involved. So, once again, for basic excisions or biopsies or even basic hysterectomies, it is adequate.
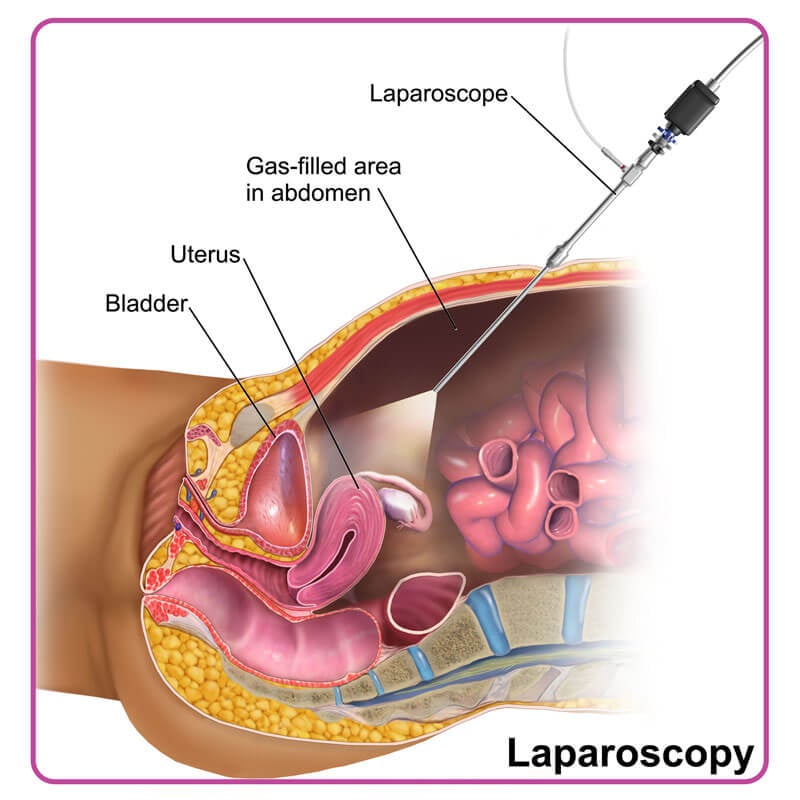
For more advanced surgery losing that 3-D third dimension is like operating with one eye closed. You lose the depth perception that is very important for delicate surgery in difficult spaces. Try closing one eye and doing things around the house. It’s harder to do isn’t it? Picking things up is not as exact. You can certainly compensate, as people do when they lose an eye, but it’s harder to judge what is further from or closer to you. So, given a choice, using both eyes is better and 2-D laparoscopy screens mimic having one eye closed. This is part of why robotic surgery adds safety to endometriosis excision.
Robotic Surgery Excision
Robotic surgery for treatment of endometriosis by excision is the 21st century tool of choice. It is laparoscopy on steroids, so to speak. While there are expert laparoscopists who argue that robotic surgery does not add anything beyond laparoscopy, the arguments used are usually cost-benefit business-related mumbo jumbo, some of which is only true when centers are not used to using robotics. But this is not your problem anyway. You want the best equipment and the best surgeons possible to help you beat endo. Robotic surgery for treatment of endometriosis has many features and clinical benefits. These are only some of them:
Less tissue injury internally due to finesse wristed instruments
Less blood loss because of the instruments and better visibility
Less trauma to your abdominal wall because the instruments do not move as much
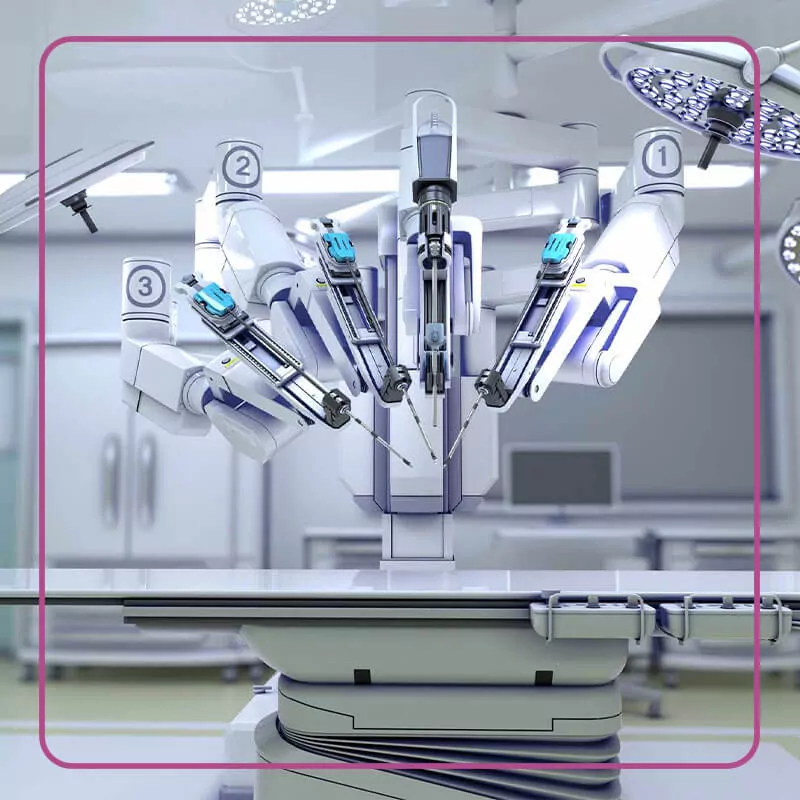
These features lead to:
Shorter recovery time
Less scarring
Fewer complications, transfusions and readmissions
Fewer “conversions” to a big incision due to inability to finish the surgery via minimally invasive approach
Better ability of surgeon to excise endometriosis

Drawbacks of robotic surgery include a slightly longer time to complete the surgery (mostly the setup time before surgery starts), it is more costly (but your co-pays are the same as laparoscopy), and it is not easy to learn. Many surgeons take robotic surgery training, but you do not want a rookie surgeon for complex endo surgery. Select wisely. We realize some studies are published which still claim no difference compared to laparoscopy. It’s important to realize that studies do not capture all the differences between patients and statistics are complex. Without video proof, it is hard to tell if the surgery was even the same quality and extent. So, as mentioned, laparoscopy is certainly a reasonable tool for many cases but do you want to take a chance that your case may be a bit too difficult for a surgeon with one eye (2-D) and without wrists (straight stick instruments)? As noted, at GOI we approach cases individually but have the robot available for your safety and best outcomes.

Medical Treatment
Medical endometriosis treatment is largely based on hormonal options and/or pain symptom management. At this time we focus on what we do best, which is our very specialized and advanced surgical help, as well as counseling about cancer risk. We will collaborate with your gynecologist or reproductive endocrinologist but do not provide medical therapy for endometriosis. If you do not have someone that can manage the medical and hormonal part of your endo care, we can help you find someone to be part of your endometriosis-fighting team!
Integrative Natural Support
For mild symptoms of endometriosis, there are integrative natural support options to consider and here is an example of some of them:
Turmeric
This spice contains a bioactive ingredient called curcumin, which is a strong anti-inflammatory. Pepper helps its absorption. It’s best to use the root or spice and just add to your salads or as part of curry dishes.

Ginger
This natural root also reduces inflammation and helps reduce nausea that may be caused by the pain of endometriosis. You can make ginger tea by boiling 1 tablespoon of grated ginger into 2 cups of water for 10 minutes. After straining it, add honey. You can also get some ginger pieces and simply chew on them as needed.

Chamomile
This natural herb from daisy-like flowers is also an anti-inflammatory. But beware that it is also a diuretic, so it can make you feel the urge to pee often. You can make chamomile tea by steeping 2 teaspoons of dried chamomile mix in 1 cup of hot water for five minutes, straining it and adding honey for sweetness if desired. Chamomile supplement capsules also exist if it’s inconvenient to make tea.

Bromelain
Bromelain is an enzyme which helps digest protein and has been used as a digestive aid and anti-inflammatory agent. It can be taken in capsule form, but fresh pineapple pulp is a great source.
Endometriosis Treatment Outcomes

Cure Rates
It is difficult to cure any disease when the exact cause is unknown. Such is the case with endometriosis. As we enter the molecular age of targeted therapy, this will change. However, today anyone with endometriosis is likely to see it recur after any medical or surgical therapy. So, the best plan is to make sure the diagnosis is correct, consider removing significant disease with minimally invasive surgery (especially deep infliltrating endo), then focus on ways to minimize estrogen excess in your body. This may include medical treatments listed above or simply being as fit and lean as you can be. Often repeat surgery is required, but you want to limit the number of times this is done to limit scarring from the surgery itself, which can also produce pain. Also, the more surgeries are performed and the more scarring (adhesions) that are potentially created, the more complications are increased. Working with a master surgeon is crucial.
What Patients Are Saying About Dr Steven Vasilev MD
Robotic Surgery Endometriosis Excision Outcomes
Regarding the surgical expertise and outcomes with robotic surgery, from focal to widespread endometriosis, we stand very unique on the West coast. The following information is crucially important in selecting your surgeon.
Basic robotic surgery training and expertise in pelvic surgery is becoming more common for many conditions, including cancer and endometriosis treatment. However, currently, radical robotic multi-quadrant excisional surgery is not standard of care because an advanced skill set for this is not sufficiently prevalent among the majority of surgeons. This expertise is slowly evolving with a relative handful of committed surgeons practicing nationally with adequate experience, who embrace the technique with strategies and tools to minimize risk of conversion to laparotomy while achieving as close to “complete” R0 or CC0 excision as possible. This “R” and “CC” based scoring is something we use for ovarian cancer when life is on the line, not just pain reduction. But the concept is the same, that being to remove the endometriosis as close to “complete” as possible.

Our surgical experience with complex and re-operative robotic surgery spans over eight years and thus far, the results include low conversion rate of <1% with a high rate of complete CC0 macro-cytoreduction and practically all achieving more than "optimal" cytoreduction status with minimal CC-1 remaining disease (almost microscopic and superficial only). In selecting your surgeon it is critically important to understand the following. While today's imaging with MRI, CT and PET-CT is good for larger disease, it is not even close to being perfect in predicting the extent of disease or distribution.
Therefore, the endometriosis distribution can be pan-abdominal and pan-pelvic, and beyond. In other words, it can be anywhere and involving any organ. Literally, ALL possible situations need to be anticipated and prepared for to optimize outcomes with the lowest morbidity (complications), lowest conversion rates to a big incision and to get the best possible resection success. We have the specialized tools and advanced expertise to provide a very unique surgical benefit to you even in very advanced endometriosis situations. As noted, we are not alone nationally in offering über-surgical expertise, but are in a unique position regarding the ability to provide minimally invasive surgical options, even in the face of very advanced disease.
Beyond Life With Endo
Beyond beating endometriosis there is quality of life, which can be equally as important. This is especially true because treatment beyond surgery can extend for a long period of time. To achieve the best quality of life after a diagnosis of endometriosis, a personalized treatment plan is crucial to beat your endo and thrive. In addition, the treatment plan must evolve as time goes on. By focusing on you as an individual, and not just on your disease, we guide you every step of the way. We specialize in helping you plan out the best outcomes possible based not just on your endometriosis but also on your body, mind and spirit.
What Patients Are Saying About Dr Steven Vasilev MD
Steven A. Vasilev MD Biography
“I help and guide women to defeat gynecologic cancers, endometriosis and complex gynecologic conditions using a unique combination of minimally invasive robotic surgery, precision cancer therapies and complementary holistic natural support towards thriving in survivorship.”
Dr. Vasilev is the only physician quadruple board certified in Ob-Gyn, Gynecologic Oncology and Integrative & Holistic Medicine in the United States. He is an accomplished oncologic and robotic surgeon and has trained hundreds of fellows and residents. Currently, he serves as Medical Director of Integrative Medicine and Integrative Gynecologic Oncology at Providence Saint John’s Health Center, Professor at Saint John’s Cancer Institute in Santa Monica, California and is Clinical Professor at Loma Linda University School of Medicine.
His residency and fellowship, leading to double-board certification, included extensive training in surgery not only on gynecologic organs but also bowel, bladder, ureters, diaphragms and all other organs in the abdomen and pelvis that can be affected by cancer, endometriosis and related conditions. This, combined with over three decades of experience in advanced minimally invasive surgery, allow him to safely complete very advanced surgeries with a very low complication rate, which is a matter of record.
Since completion of his fellowship training in Gynecologic Oncology at the USC Kenneth Norris Comprehensive Cancer Center he has been recognized as a surgical innovator, minimally invasive surgery pioneer (among first group in the US to regularly perform complex laparoscopic surgery such as radical hysterectomy and lymph node dissection in the late 80’s and early 90’s), and thought leader. He has held multiple leadership positions and been on the faculties of Kaiser Permanente, City of Hope, UC Irvine, USC, UCLA and Loma Linda University.
Dr. Vasilev has been involved in running research programs at multiple sites since 1977. He is a sought-after speaker, has authored over 90 publications, abstracts, book chapters and is the author-editor of a gynecologic oncology textbook and a popular book on integrative oncology.
His research is in surgical innovation, novel cancer theranostics, and integrative & complementary health. He is an active member of multiple medical societies and has been nationally listed in “Best Doctors” for 20 years.
His clinical focus is on ovarian masses/tumors, cancer and endometriosis.
Steven Vasilev MD holds an MBA from UCLA, with training in, and work history of, process improvement in organizational change using tools like Lean Six-Sigma and TOC. You can discover much more about Dr. Vasilev by visiting his personal website: StevenVasilevMD.com
Center of Excellence
Dr. Steve Vasilev is a world-renowned surgeon and endometriosis specialist who focuses on robotic endometriosis excision surgery for all of the reasons noted in this article, including his personal touch with holistic natural support that includes proactive lifestyle guidance and nutritional counseling guided by your unique needs. All newly diagnosed patients seeking treatment options should contact him because he offers an integrative approach tailored specifically to you!
The Institute, located in Santa Monica, California, focuses only on advanced cancer and complex benign conditions such as endometriosis excision surgery. We match your needs, based on case complexity and underlying cancer risk, with the right surgical team.
Dr. Steve Vasilev supports endo surgeons, mainly for re-operative and advanced endometriosis excision surgery. He is a renowned expert in complex pelvic and abdominal minimally invasive robotic surgery and has been performing advanced minimally invasive procedures, both laparoscopic and robotic, since 1988. In 1990 he was one of a handful of advanced laparoscopic surgeons already performing minimally invasive radical cancer surgery, above and beyond endometriosis surgery.
Personalized High-Tech Endo Excision
Endometriosis is highly variable in extent and location, so you want personalized treatment options. Just like diseases differ, so do individuals and their specific situation. We have the highest tech and the most advanced surgical skill-set, but individual needs call for different answers to help you defeat endo and thrive. ~Dr. Steve Vasilev
.webp)
Steven A. Vasilev MD Awards

Best Doctors
Dr. Vasilev has been nationally listed in “Best Doctors” for 20 years.
.png)
Quadruple Board Certified
Dr. Vasilev is the only physician quadruple board certified in Ob-Gyn, Gynecologic Oncology and Integrative & Holistic Medicine in the United States.

Super Doctor 2022
Dr. Vasilev is selected as a Super Doctor 2022 in Gynecologic Oncology and Pelvic Surgery.
Dr Steve Vasilev’s Research, Publications & Books
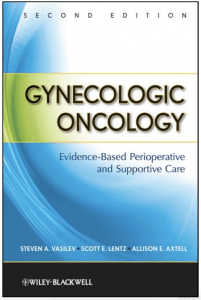

Dr Vasilev is extensively published and according to Academia.edu his work has been cited by other professionals and colleagues hundreds of times, meaning he is a respected national expert on multiple topics related to cancer, minimally invasive surgery, peri-operative recovery and integrative medicine.
OFFICES:
Gynecologic Oncology San Luis Obispo
Gynecologic Oncology Los Angeles Gynecologic
Oncology Beverly Hills Gynecologic Oncology
Santa Monica Gynecologic Oncology Marina del Rey
Centers:
Endometriosis Excision
Ovarian Cancer Cytoreduction
Robotic Surgery
Uterine Cancer /Hysterectomy
Cervical Cancer
Complex Gynecology Surgery
Ovarian Cysts